Department Introduction
Department of Anesthesiology | Our Speciality
:::

Unlike conventional sedation anesthesia, the department adopts the highest safety standard. In addition to basic vital signs, the bispectral index (BIS), the end-tidal carbon dioxide and the respiratory frequency monitoring were also added, allowing children to receive dental treatment in a comfortable and safe condition.

Our Speciality
Sedation anesthesia without intubation at the pediatric dentistry

Aimed at the children afraid to go to the dentist, the department has created a personalized sedation anesthesia program. Compared with general anesthesia with conventional intubation (breathing tube), the professional team steps in for anesthesia and pediatric dentistry. The latest drugs and instruments are used for monitoring so that children’s fear can be dispelled, including offering health education before anesthesia, dental clinic care, and matters needing attention after returning home, which are all covered within the scope of care.
Unlike conventional sedation anesthesia, the department adopts the highest safety standard. In addition to basic vital signs, the bispectral index (BIS), the end-tidal carbon dioxide and the respiratory frequency monitoring were also added, allowing children to receive dental treatment in a comfortable and safe condition.
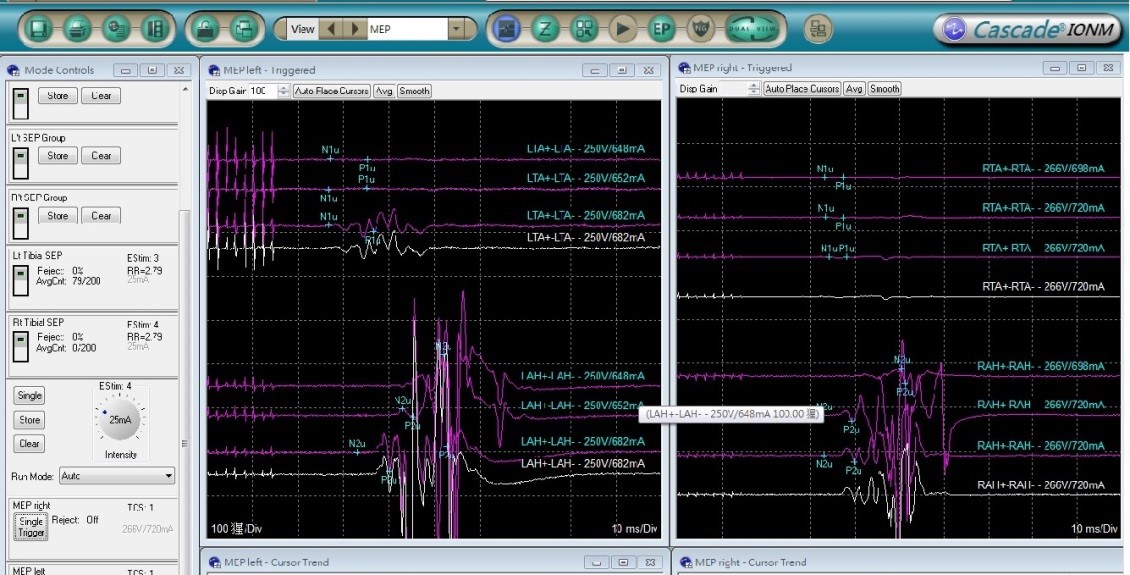
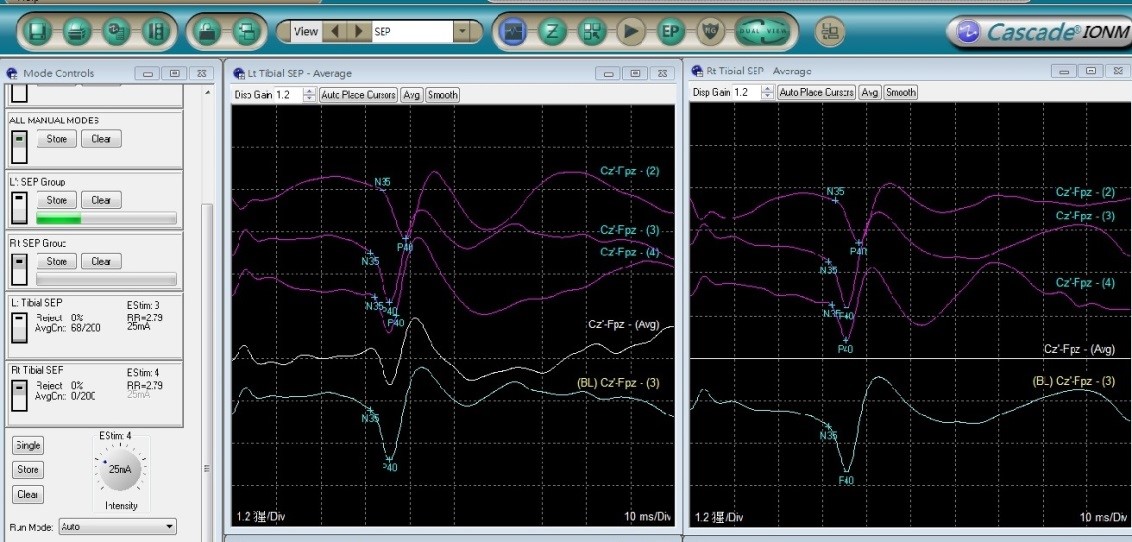
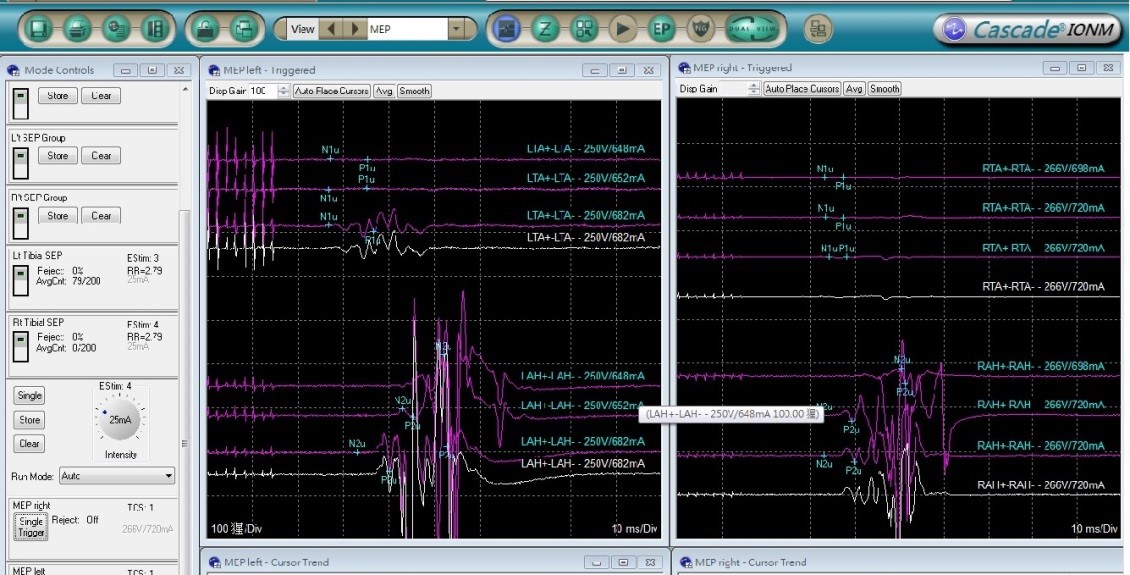
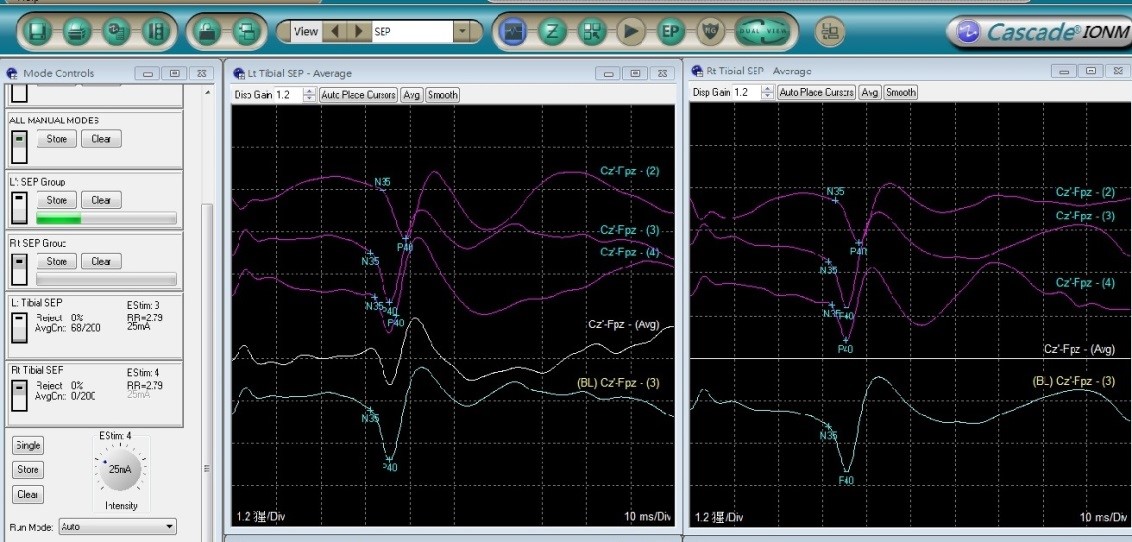
Spinal surgery and evoked potential monitoring
Scoliosis surgery may cause nerve damage. Conventional nervous system monitoring performs "wakefulness testing" during the surgery. The disadvantage is that the sensory nerve cannot be tested, and the anesthesiologist and the patient must ensure that during the testing, the patient is not restive after being awake and follows the doctor's instructions to complete the examination. It is not applied to all patients.
The evoked potential monitoring (including somatosensory and motor evoked potential) is used in the hospital for examination with a 16-channel nerve monitoring instrument and a 10-20 system. The principle of the evoked potential examination is that when the nervous system receives stimulus, it will cause changes in electrical activity. By recording these changes via machines and transforming them into waveforms, we can check whether there are abnormalities in the nerve conduction pathway, in an effort to provide perfect monitoring of scoliosis surgery and to make the operation safer.
Intravenous general anesthesia

The department has abundant experience in intravenous general anesthesia for precise examination and treatment of the liver, gallbladder, and stomach and intestines, with a good safety effect. The department can assist part of examinations, including checkups, gastrointestinal endoscopy, percutaneous liver tumor cauterization, transesophageal echocardiography, and special radiography. We have a specific attending anesthetist who completes the detailed assessment process before performing anesthesia. Moreover, with advanced target anesthesia machines and perfect environment and devices at medical center level, adverse reactions, such as abdominal distention, pain, anxiety, and stress arising from the examination or treatment are greatly alleviated during anesthesia. It not only enables subjects or patients to feel highly comfortable and satisfied, but also helps to ensure the precise implementation and safety of examination and treatment.
Surgery for catheter-based aortic valve replacement
Surgery for catheter-based aortic valve replacement is a new treatment for aortic valve stenosis and a minimally invasive interventional therapy, through which the catheter is put into the heart via the inguinal incision and the originally narrow aortic valve is stretched through the valved stent, so that the implanted valve can replace the originally narrow valve and return to normal operation. The treatment is performed by teamwork in a cardiac catheterization room or in a hybrid operating room. The anesthesiologist needs to not only put patients under general anesthesia to assuage their discomfort and anxiety, but also work closely with cardiologists (or cardiac surgeons) in monitoring the physiological status of the patient at all times. In addition to blood pressure and heartbeat, cardiac output can be obtained through new monitoring instruments. Cardiac output provides more physiological parameters for operating doctors as well as positioning through the transesophageal cardiac ultrasound assisted valve placement. Due to the influence of anesthetic drugs on the cardiovascular system, we also provide anesthesia depth monitoring equipment, giving more precise anesthesia depth and stability, so as to cushion the effect of the drugs and promote recovery.
Bariatric surgery
The target of bariatric surgery is morbidly obese patients. Such patients have a weight problem which poses a bigger challenge than general surgery with respect to anesthesia. As the patients are heavier, their neck circumference is larger, and the proportion of the soft tissue in the mouth is higher, it is very difficult to induce the establishment of the airway by anesthesia. The department currently has a number of image-based airway devices, allowing anesthesiologists to properly set up a respiratory tract and exempting obese patients from the risk of hypoxia while building an airway. Obese patients have excess body fat. The commonly used anesthetic gases are highly liposoluble, making the patient more prone to accumulate anesthetic drugs during surgery which is disadvantageous to recovery. The department is equipped with anesthesia depth monitoring instruments which can provide accurate depth of anesthesia and avoid excessive accumulation of narcotic drugs. In addition, the best muscle relaxation auxiliary device applied during the operation can allow patients to relax and giving muscle relaxant antagonists at the end of it can enable the muscle strength to quickly return to the preoperative state, remove the respirator early, and shorten the recovery time of anesthesia.
▲
