Chest Pain Center and Acute Myocardial Infarction (AMI) Care
▪ Established in 2009, our Chest Pain Center provides 24/7 year-round medical services. In 2019, we introduced an AI-assisted system in the emergency department to enhance AMI patient care efficiency. In 2023, our median Door-to-Balloon (D2B) time was 51 minutes, significantly below the international standard of 90 minutes.�
▪ The center has received the National Biotechnology and Medical Quality Award for four consecutive years and is accredited by the Joint Commission of Taiwan for AMI, coronary artery, and heart failure care quality.
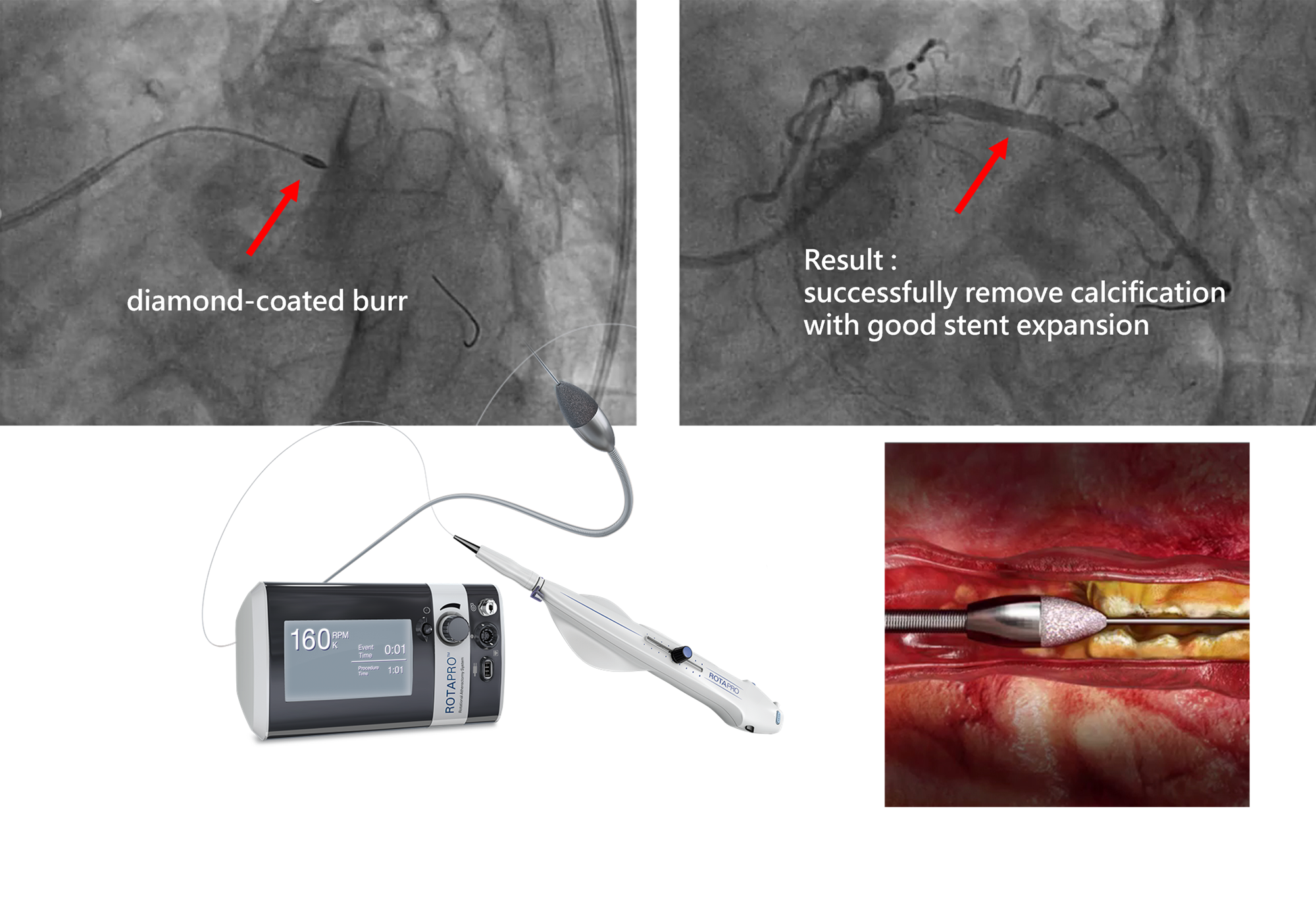
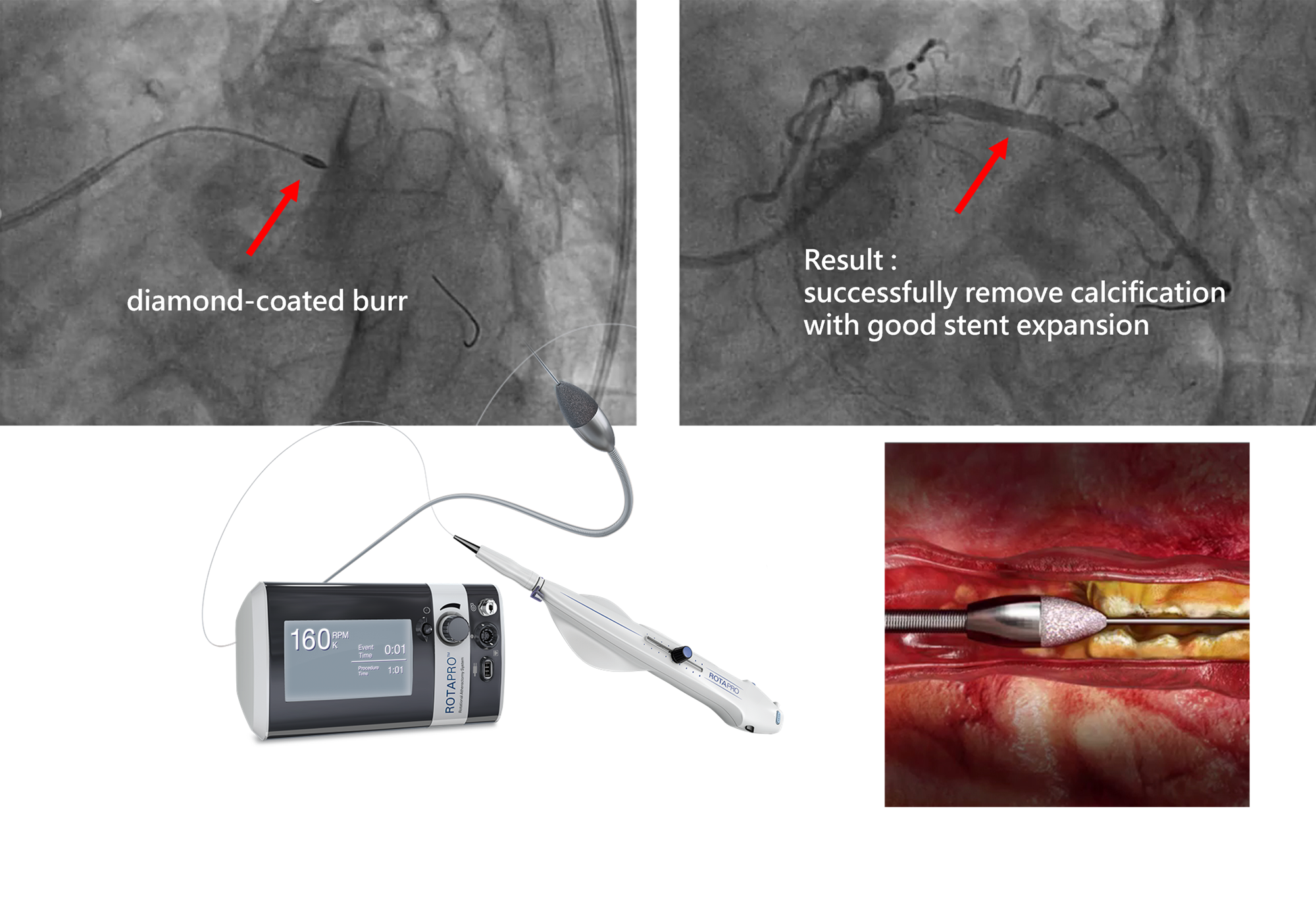 Coronary rotational atherectomy
Coronary rotational atherectomy :Uses a diamond-coated burr to modify severe coronary calcifications, ensuring optimal stent placement.
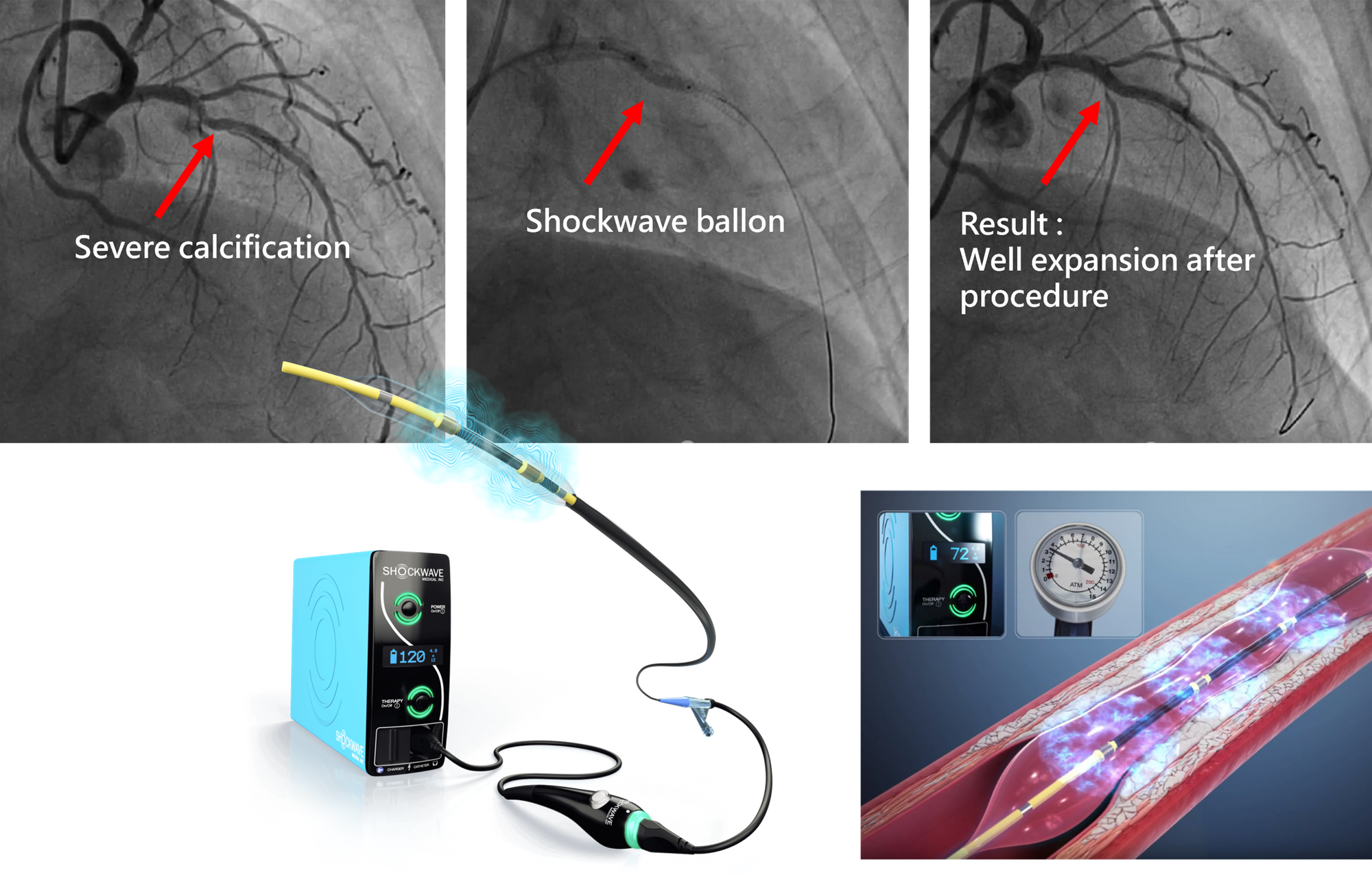
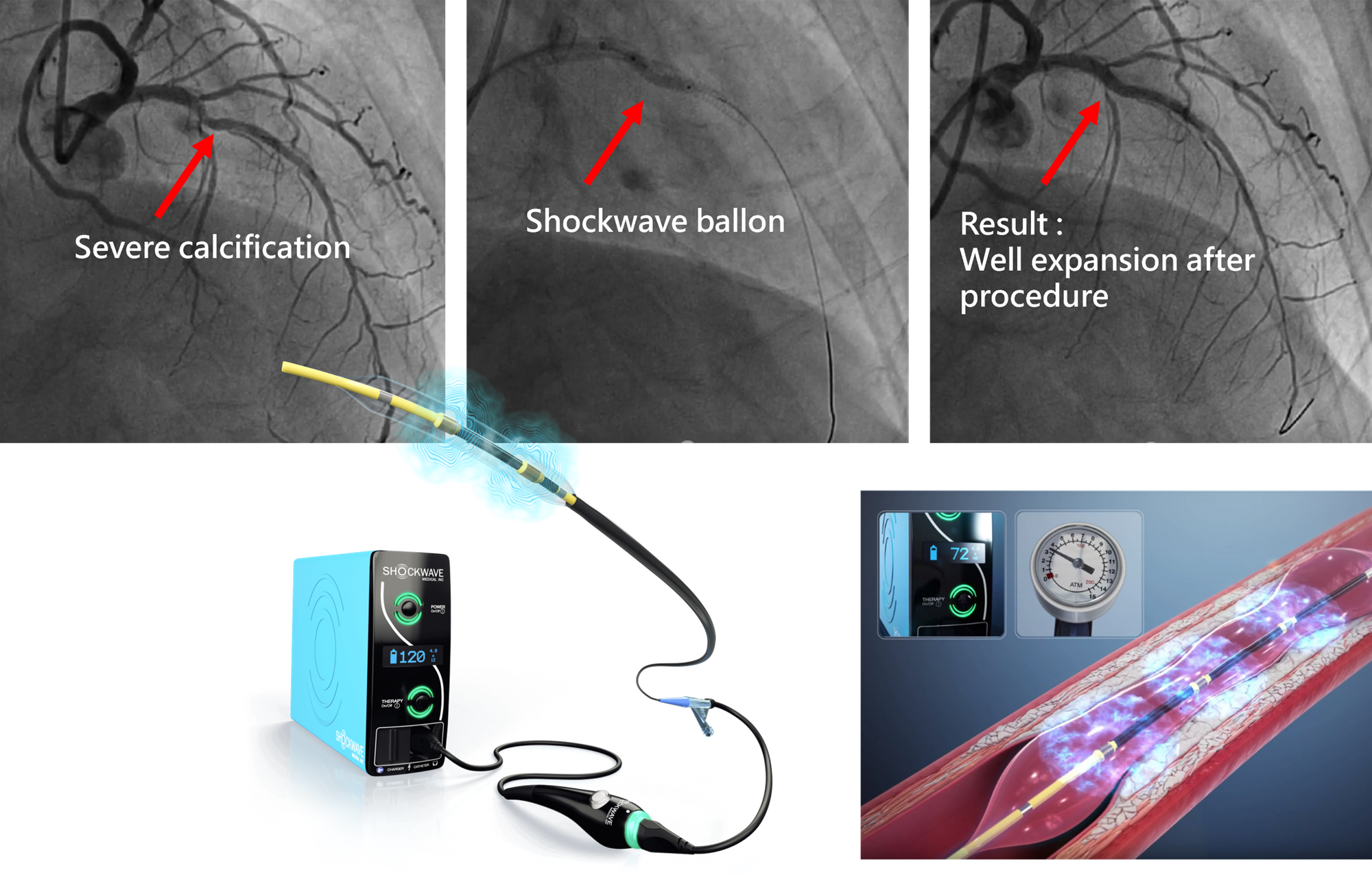 Shockwave intravascular lithotripsy
Shockwave intravascular lithotripsy :An innovative, catheter-based therapy that uses acoustic wave technology to safely fracture severe coronary artery calcifications, facilitating optimal stent expansion and improving blood flow.
Coronary Artery Interventions
▪ Performing approximately 2,200 cases annually, ranking among the top three nationwide.
▪ Comprehensive minimally invasive interventions for complex coronary artery diseases, including chronic total occlusion (CTO), high-risk lesions, and calcified lesions.
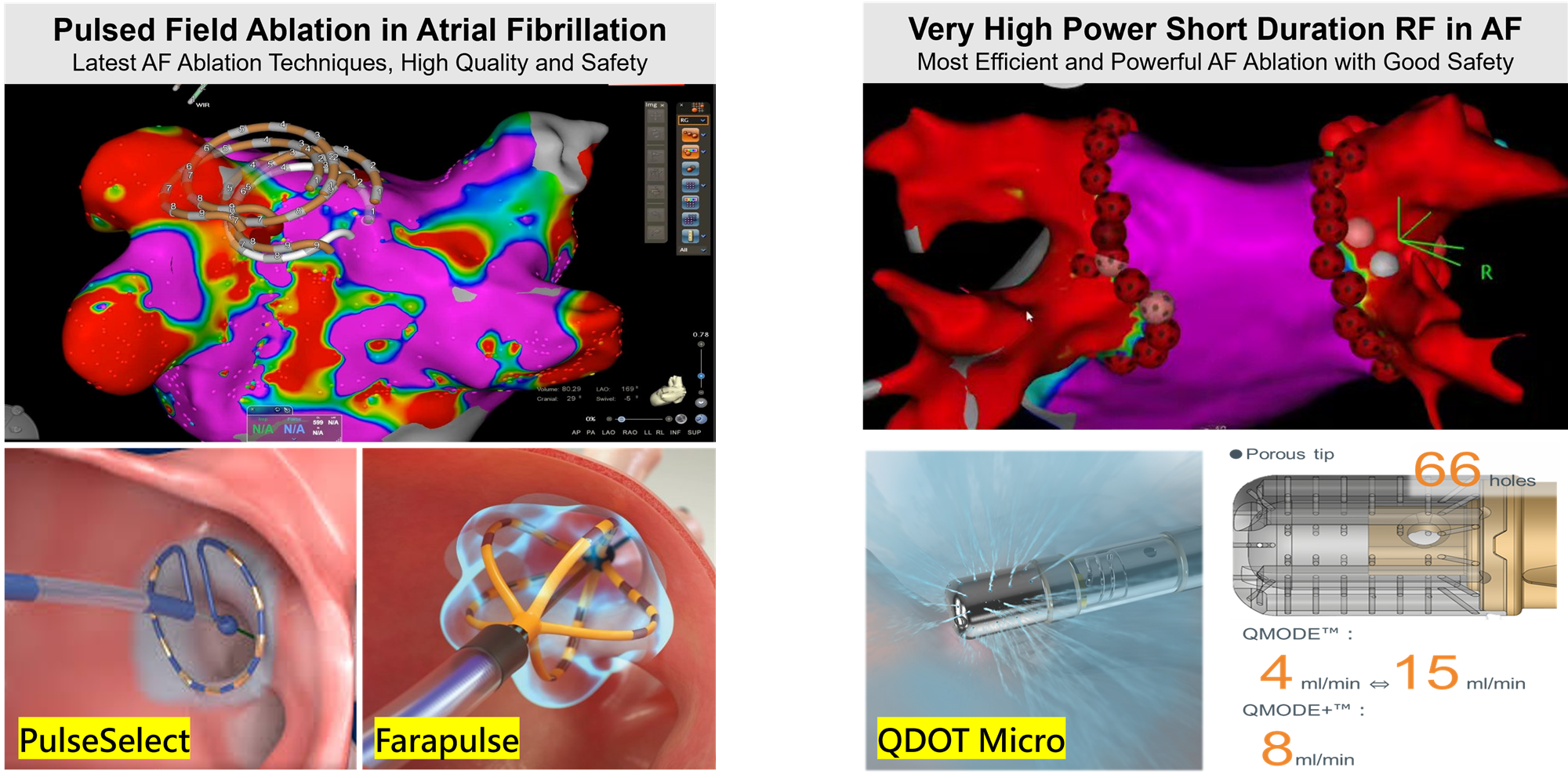
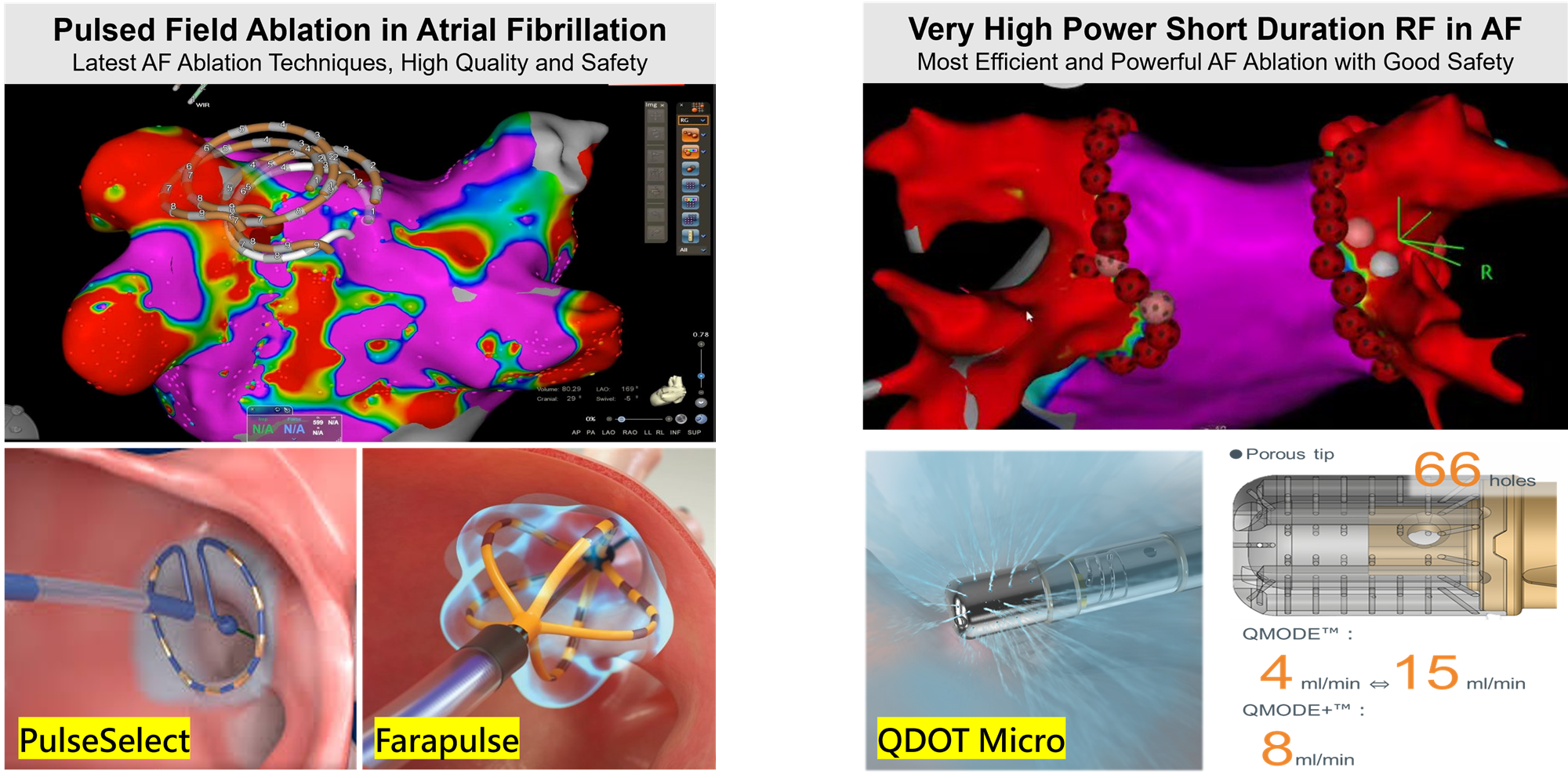
Arrhythmia and Atrial Fibrillation Treatment
▪ 3D Mapping-Guided AF Ablation : 1,775 cases completed by 2024, maintaining world-class standards.�
▪ New/Physiological Pacemaker Implantation : 601 cases performed by 2024, the most extensive experience nationwide.�
▪ One-Station AF Treatment : Combining AF ablation and left atrial appendage occlusion with preoperative 3D imaging analysis developed in-house, enhancing surgical precision, reducing stroke risk, and minimizing anticoagulant use. A total of 40 cases performed, leading the nation.
▪ 2024/10/29 First case of pulsed field ablation with PulseSelect on atrial fibrillation in APAC
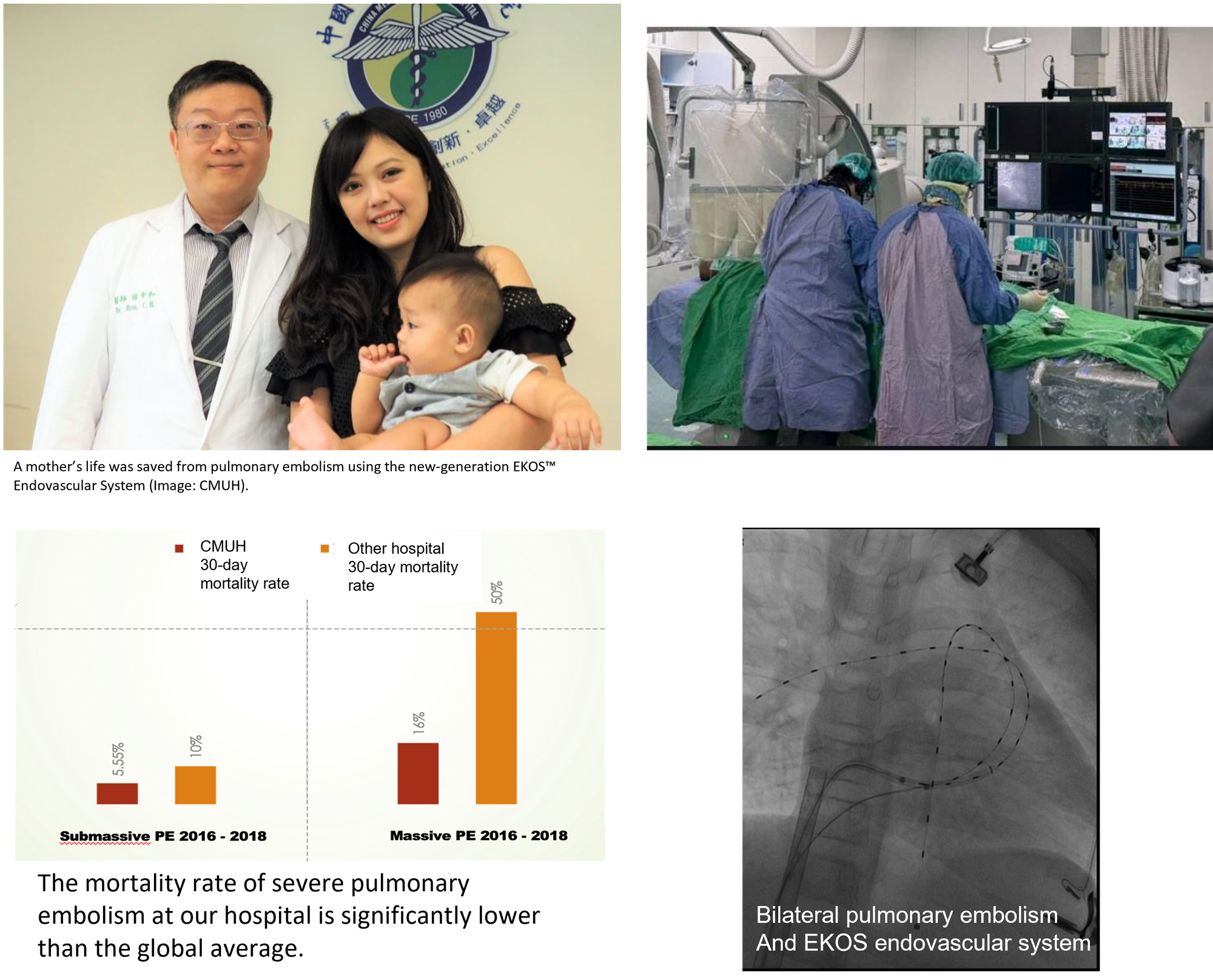
Peripheral Vascular and Thrombus Treatments
▪ EKOS Ultrasound-Assisted Thrombolysis : The first 24/7 acute thrombolysis team in Taiwan since 2016, with 927 procedures completed by October 2024, leading the nation.�
▪ Acute Peripheral Artery Occlusion : Over 800 cases using first-generation EKOS thrombolysis and more than 50 cases with second-generation thrombectomy, avoiding traditional surgery and improving success rates.
▪ Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) : Immediate thrombolysis reduces cardiopulmonary failure and thrombotic complications.
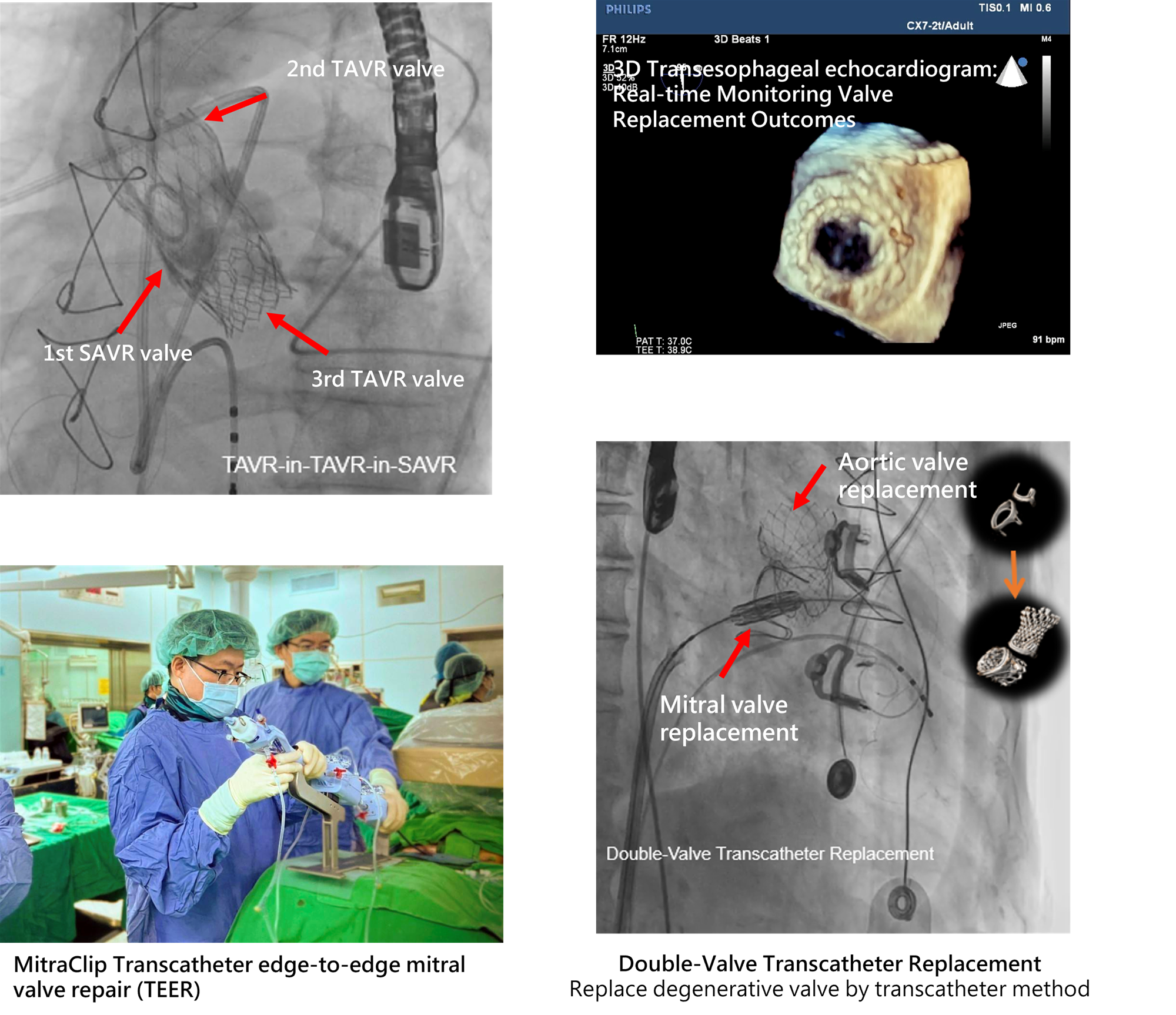
Minimally Invasive Heart Valve Treatments
▪ Transcatheter Aortic Valve Implantation (TAVI) : 96 cases completed, providing a minimally invasive alternative to open-heart surgery.�
▪ Minimally Invasive Mitral Valve Repair (MICS MVR) : 5 cases completed, including the nation’s first combined procedure with left atrial appendage occlusion.
▪ Future Developments : Introduction of transcatheter mitral and tricuspid valve replacement to expand minimally invasive options for valvular disease and improve patient quality of life.
▪ Transcatheter Aortic Valve Replacement (TAVR) : A minimally invasive procedure that avoids open-heart surgery and reduces procedure time.
Heart Failure and Heart Transplantation
▪ In 2023, we performed 41 long-term left ventricular assist device (LVAD) implantations, 42 extracorporeal membrane oxygenation (ECMO) procedures, and 52 heart transplants, ranking among the top in the country.
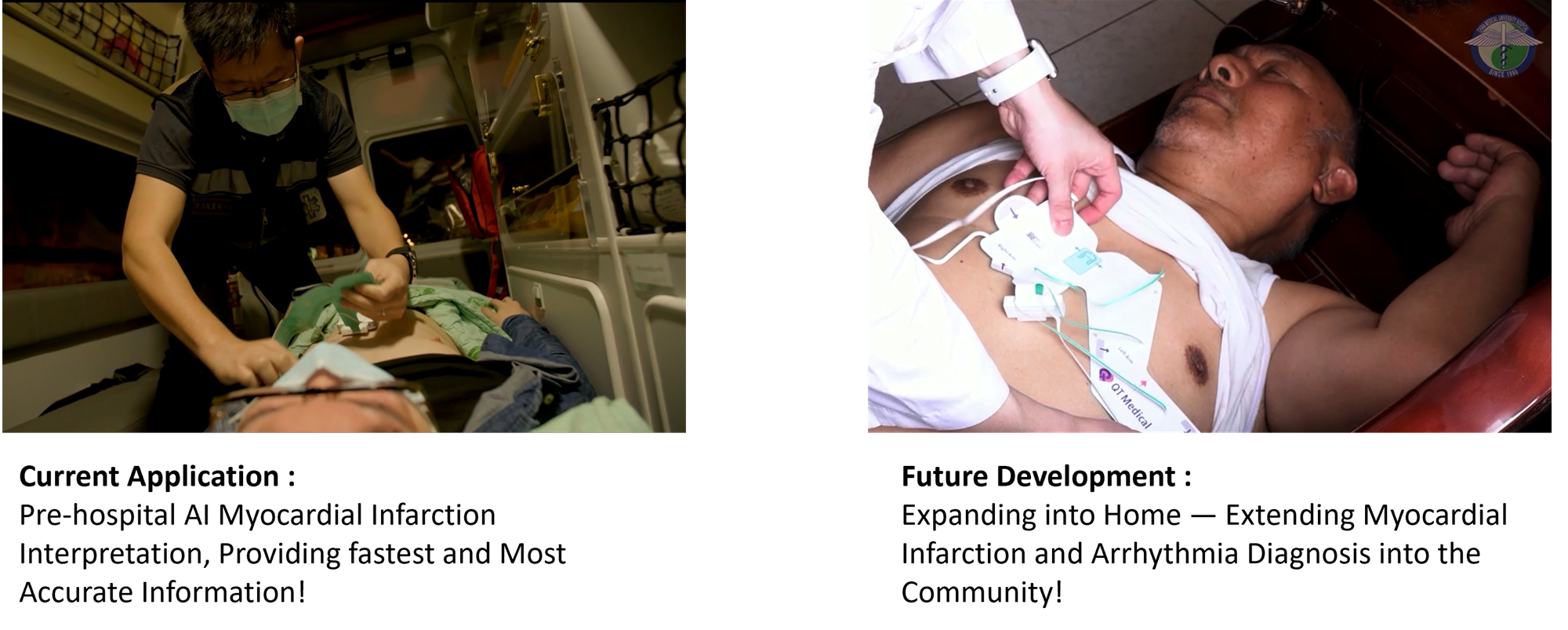
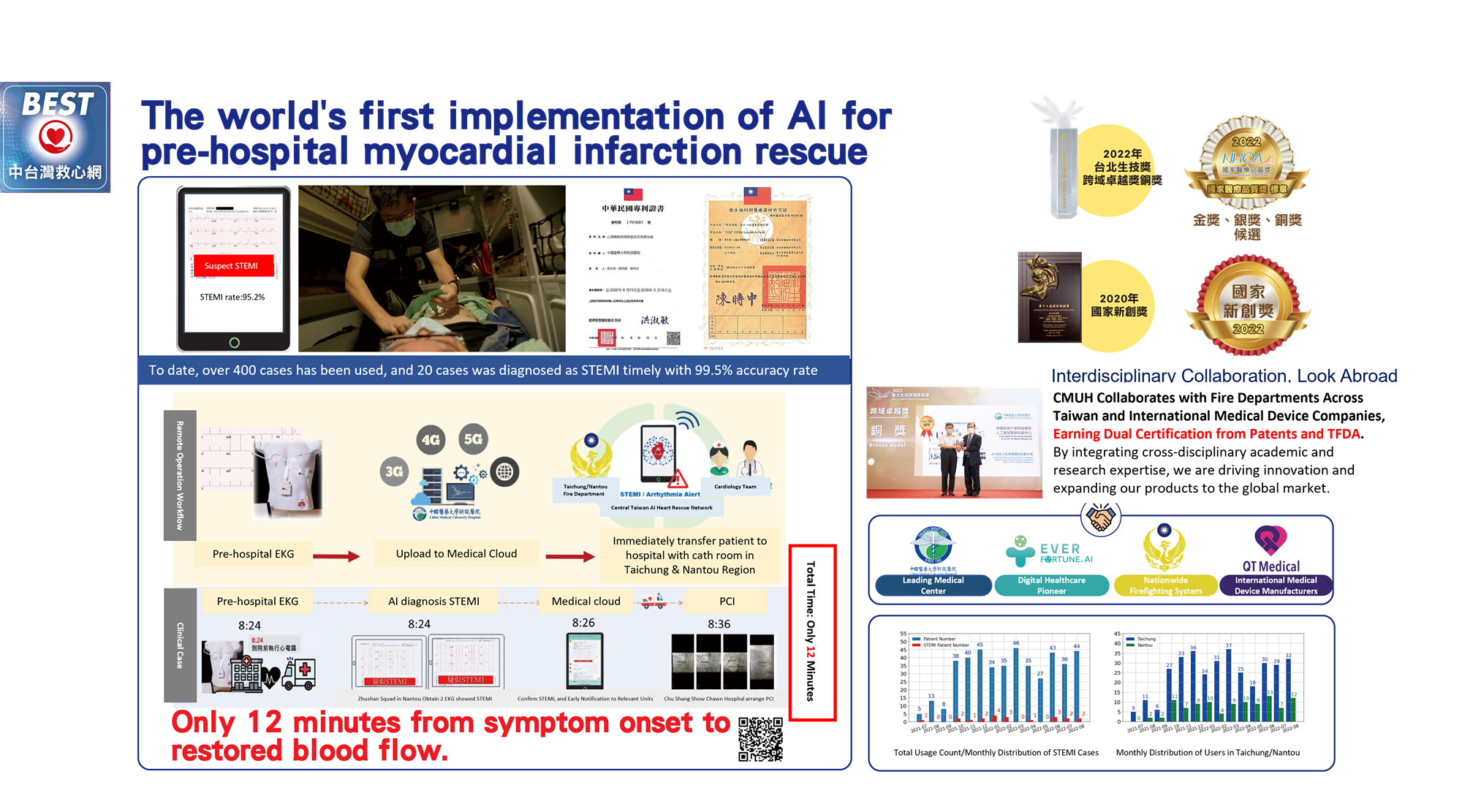
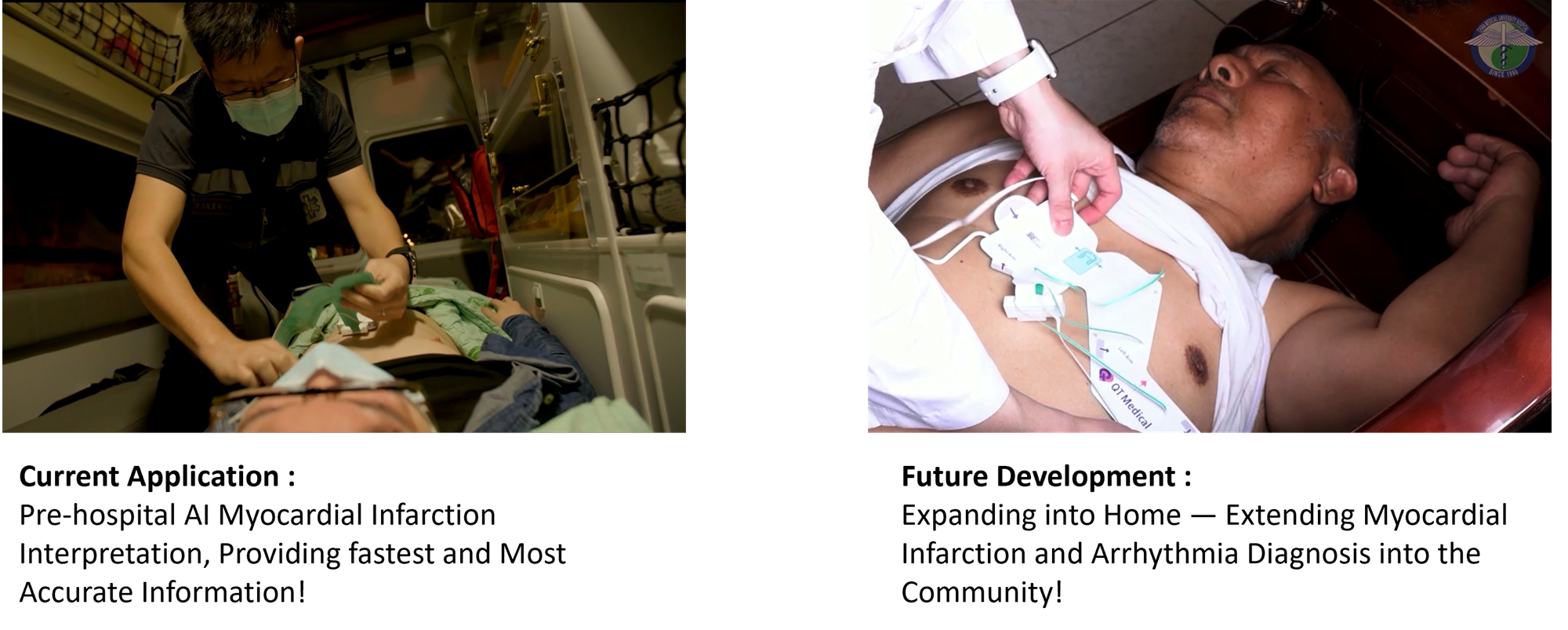
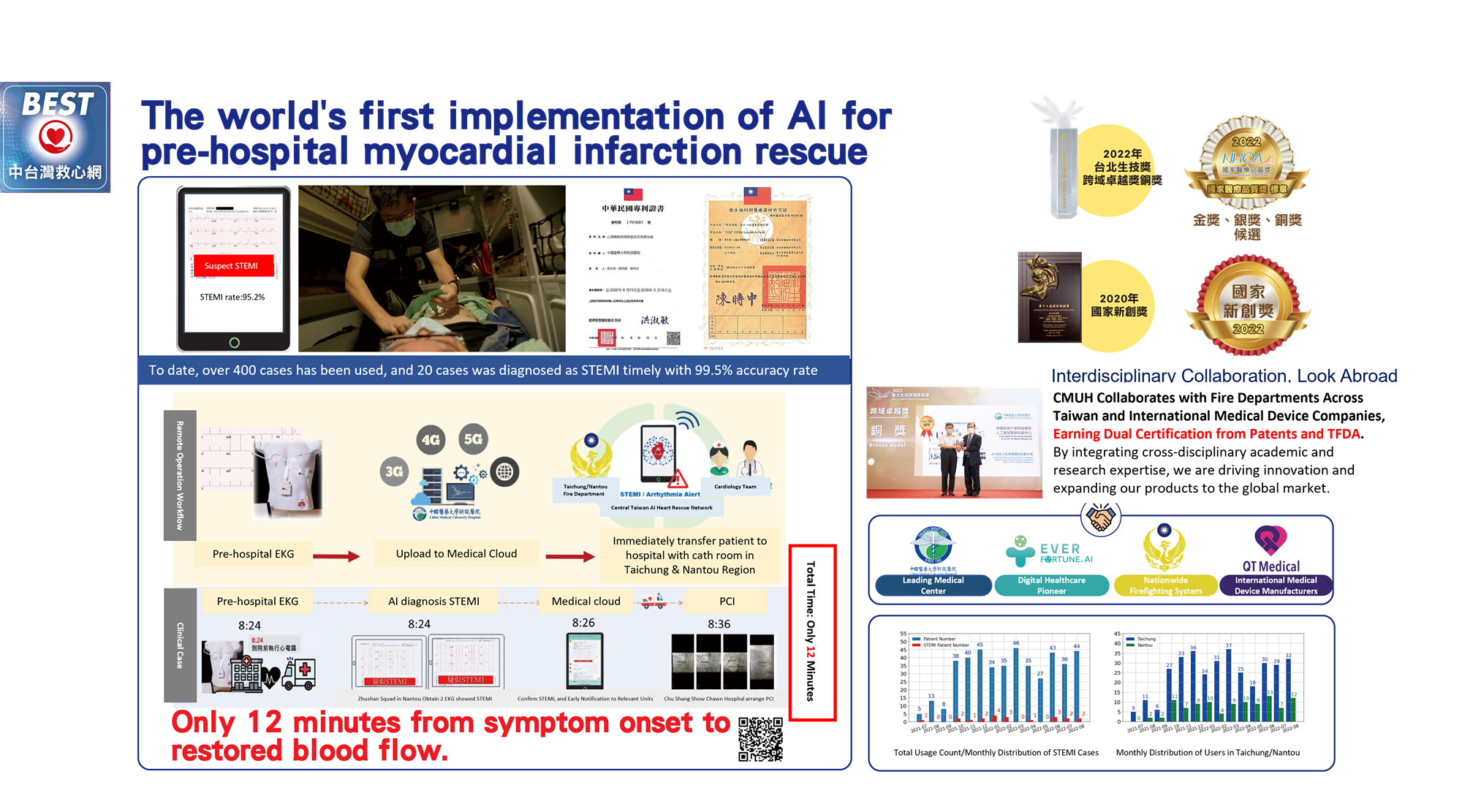
Central Taiwan AI Heart Rescue Network : Bringing AI Healthcare into the Community!
Pre-Hospital Myocardial Infarction Rescue: AI Implementation in Emergency Care.
Our center is at the forefront of applying Artificial Intelligence Electrocardiography (AI-ECG) technology in emergency care and pre-hospital rescue, enhancing the real-time detection and treatment efficiency of ST-elevation myocardial infarction (STEMI). By automatically analyzing 12-lead ECGs, AI-ECG enables rapid STEMI screening and immediately alerts physicians to activate the primary percutaneous coronary intervention (PCI) protocol. This technology is deployed in emergency rooms and ambulances, ensuring that ECG analysis and transmission are completed before the patient reaches the hospital. Clinical trials have demonstrated that AI-assisted diagnosis reduces physician response time by over 50%, significantly improving patient outcomes and ushering in a new era of smart healthcare.
Innovative Cardiac Pacemaker and Defibrillator Implantation: Leaded, Leadless, and Subcutaneous Systems

Advanced High-Energy and Pulsed Field Ablation for Atrial Fibrillation
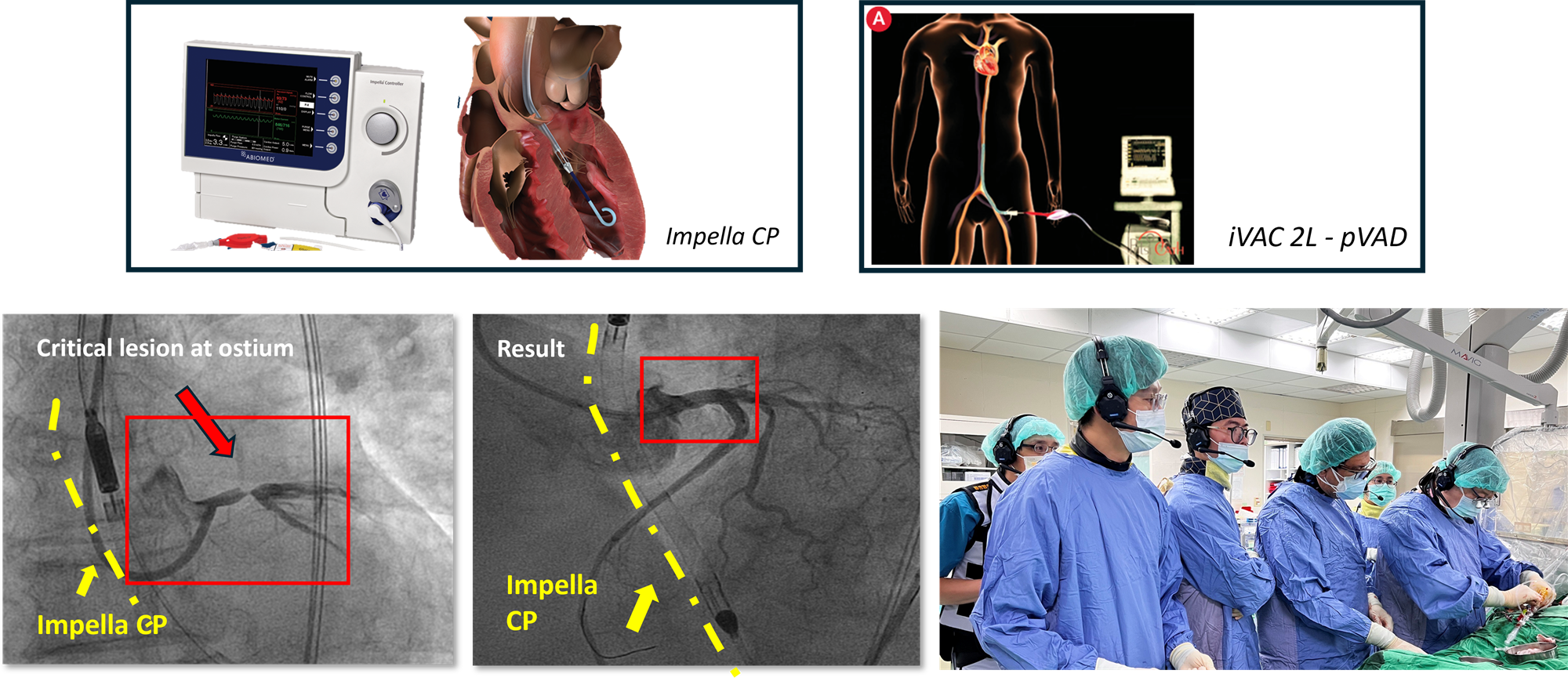
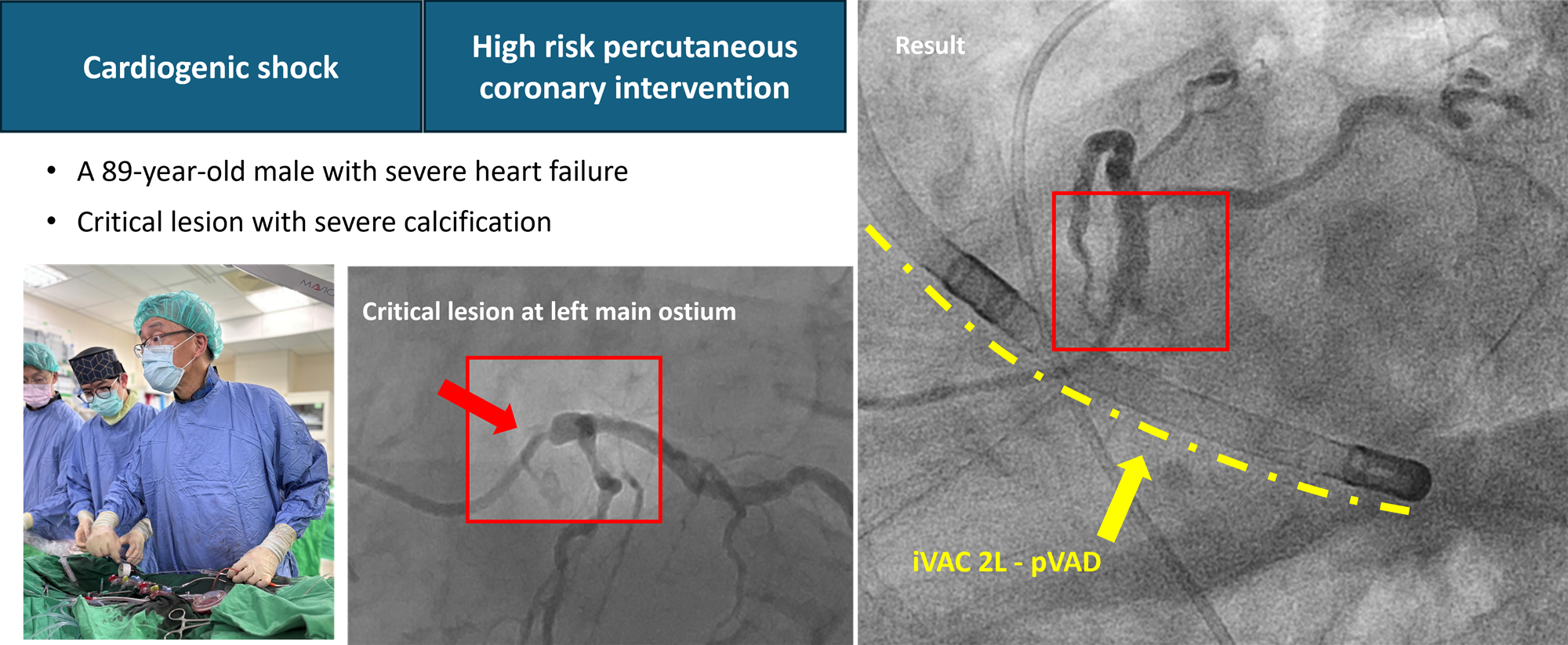
Mechanical Circulatory Support in High Risk PCI
Our center has introduced a new Mechanical Circulatory Support system to enhance the safety and success rates of high-risk coronary interventions. We utilize percutaneous ventricular assist devices (pVADs) such as Impella or IVAC to maintain cardiac output during procedures, reducing the risk of low perfusion and hemodynamic instability. This technology is particularly beneficial for patients with left ventricular dysfunction, impending cardiogenic shock, or other high-risk conditions.
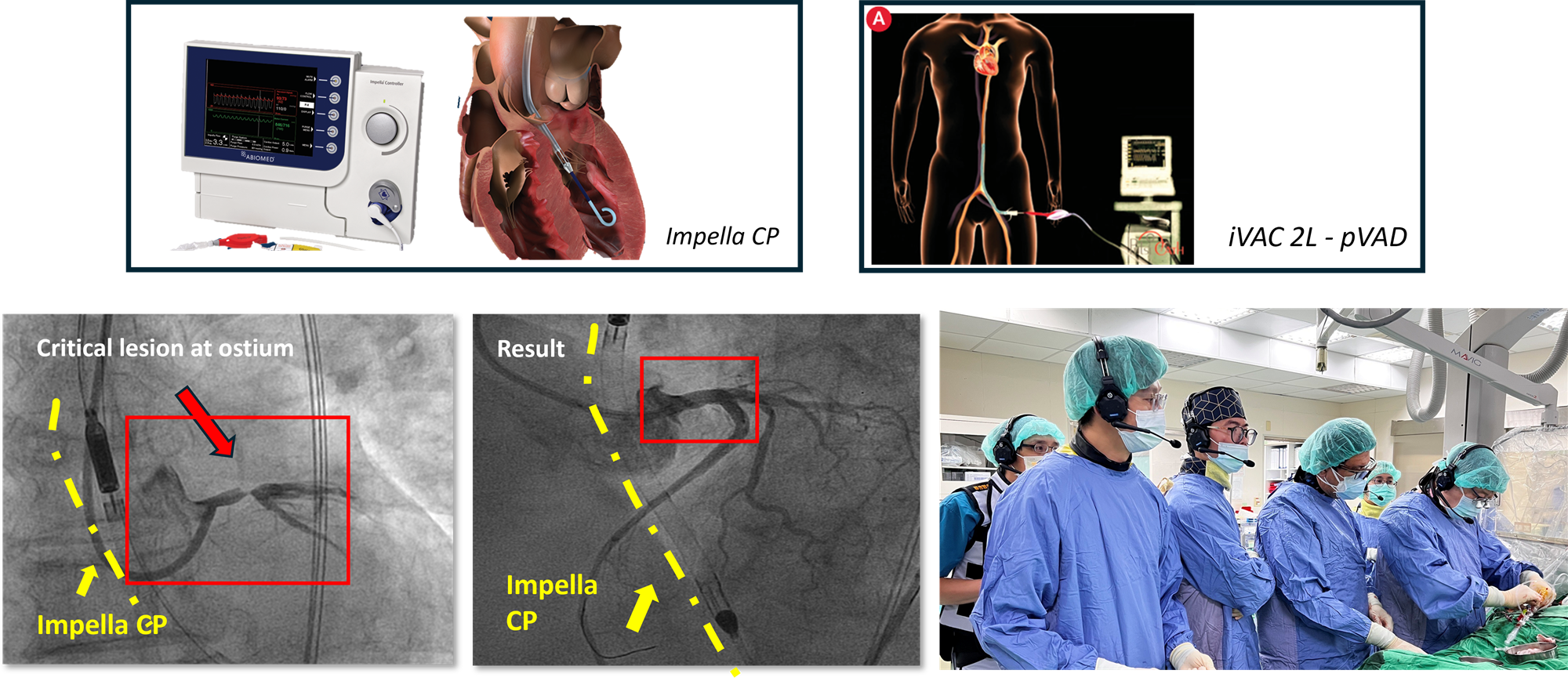 Advanced range of mechanical circulatory support options to enhance patient outcomes and procedural safety
Advanced range of mechanical circulatory support options to enhance patient outcomes and procedural safety
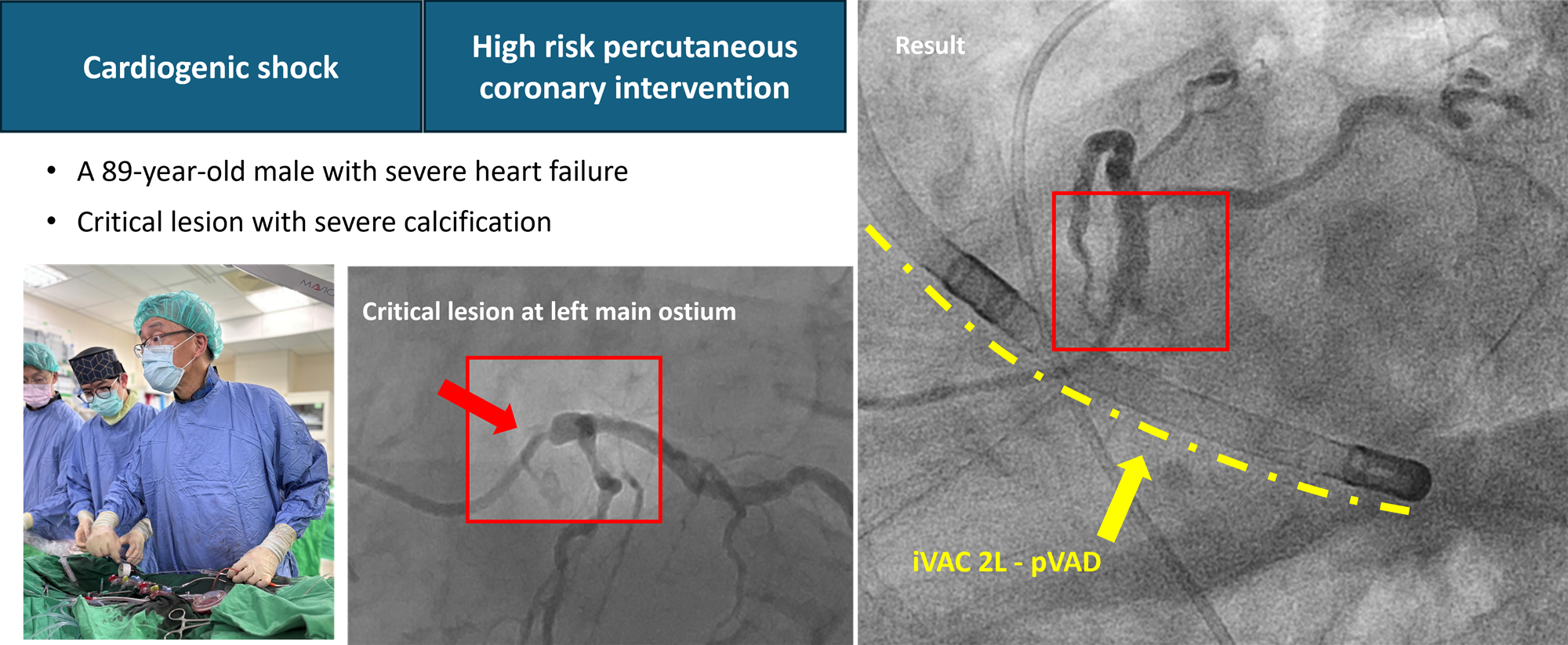 New and Advanced Support for the Coronary Intervention of High Risk Patients
New and Advanced Support for the Coronary Intervention of High Risk Patients